Strengthen pelvic floor muscles to address a major cause of incontinence
InControl tackles the problem - not just the symptoms
Female incontinence
Up to 37% of Australian women (or more than 3 million women) suffer from some degree of urinary incontinence - and 70% of that enormous number do not seek advice or treatment for their problem. This means that more 2 million women are suffering in silence!
Female pelvic floor muscles play a critical role in urinary control. A large proportion of these women could turn their uncomfortable situation around. All it requires is a short term commitment to a simple program to strengthen their pelvic floor muscles.
Manual exercise is possible for some - while others may need a little extra help with mild electrical stimulation from a small medical device. It is non-invasive, painless and inexpensive. Most important of all, it tackles the problem not the symptoms.
Diagnosis comes first
Female incontinence may be caused by a range of serious health issues. If you are unsure of the cause of your incontinence we strongly advise that you speak to your doctor to seek diagnosis.
Only when it is confirmed that weakened muscles are the cause (or possibly the partial cause) of your leakage problem, then our InControl medical device may be of significant help.
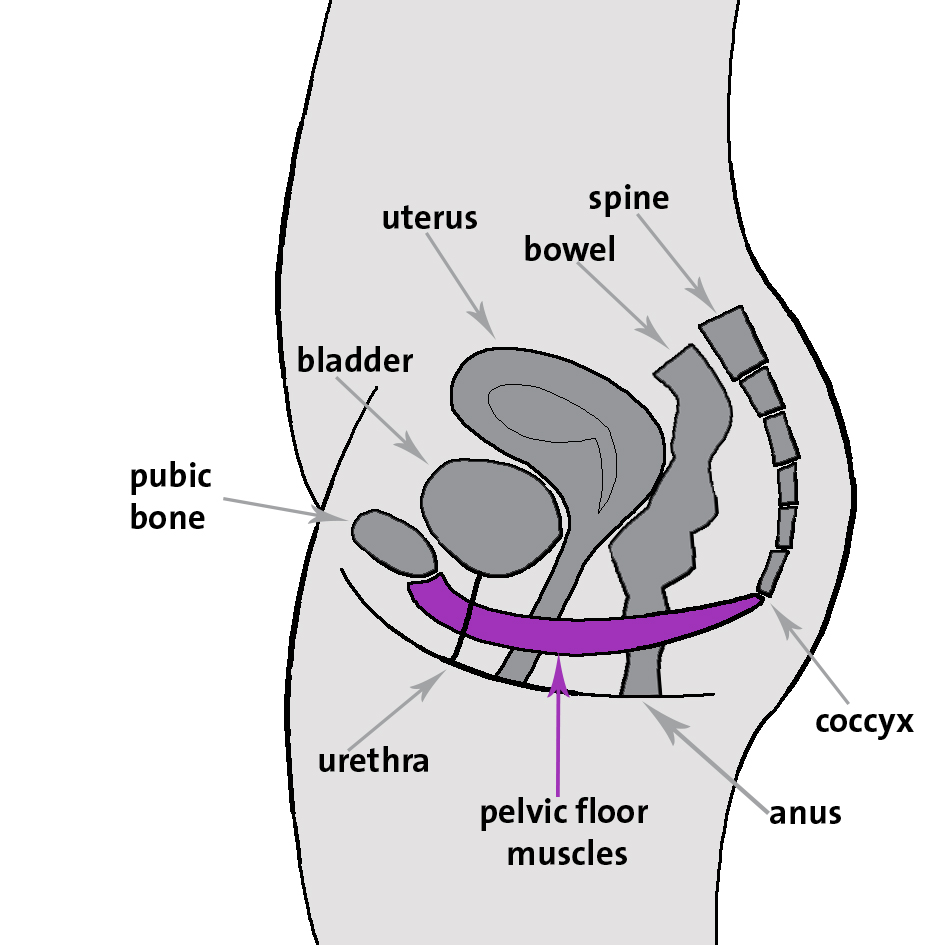
Female pelvic floor anatomy
The pelvic floor muscles are situated at the bottom of the pelvis, in a roughly horizontal orientation to support the pelvic and abdominal organs. There are three openings in women: the urethra, the vagina and the anus.
Functions of the female pelvic floor
The functions of the pelvic floor are numerous and important. They include:
Regulating continence, by opening and closing the urethra and anus
Constricting the vagina
Supporting the organs of the pelvic cavity - the uterus, bladder and bowel
Making an essential contribution to core strength. The pelvic floor is the centre of gravity in your frame - as part of your core muscles it makes a fundamental contribution to movement, back strength and stability
Playing an essential role in the sexual response - possessing well-developed and fit vaginal and pelvic floor muscles is an asset in the bedroom
Nerve supply to pelvic muscles
Pudendal nerve
The pudendal nerve is the main nerve of the perineum. It carries sensation from the external genitalia and the skin around the anus and perineum, and the motor supply to various pelvic muscles
Its branches innervate most of the pelvic floor muscles and include:
The rectal nerve (inferior anal nerve)
Perineal nerve
Superficial perineal nerve
Deep perineal nerve
Dorsal nerve of the clitoris
Posterior labial nerves
Parasympathetic fibres
The parasympathetic nerve fibres of the perineum contribute to the innervation of the pelvic and genital organs. They regulate the emptying of the urinary bladder, influence motility in the rectum and, most importantly, contribute to uterine contractions.
Autonomic Innervation of the Uterus: Branches of the utero-vaginal plexus innervate the uterus, uterine tube, cervix and upper vagina. Sympathetic innervation originates in segments of the lower thoracic spinal cord. Parasympathetic innervation originates in the S2 through S4 spinal cord segments.
Ventral primary rami
The lumbar and sacral plexus contain ventral rami from spinal nerves L1-S4. They innervate the pelvic girdle and lower limbs and help to maintain core strength.
Electrical Muscle Stimulation
If you have read this far you will realize that the pelvic floor has an extensive array of muscles and connective tissues, and is richly endowed with blood vessels and nerves, making it highly responsive to assisted exercise using electrical stimulation.
It is not always desirable or necessary to stimulate the muscles directly. Rather, the first objective is to stimulate the motor nerves and sympathetic nerve fibres that supply the relevant muscles, i.e. the various branches of the pudendal nerve, the ventral primary rami and the parasympathetic fibres.
Our recommendation is to:
Place one small electrode on the perineum, i.e. the surface area between the anus and the vulva
One large electrode over the sacrum, i.e. the large, triangular bone at the base of the spine and above the coccyx
The area between the pads is large enough to cover and stimulate all the motor nerves and sympathetic and parasympathetic nerve fibres in question. Dose is determined by intensity, the number of muscle contractions per day and the number of days in the program of treatment.
Continence related muscles
The pelvic floor muscles most important for maintaining continence include:
Internal and external anal sphincter muscles - they constrict the anal canal
Urethral sphincter muscle - which controls the opening and closing of the urethra
Bladder detrusor muscles - one muscle relaxes the bladder, another contracts during urination to release urine
Puborectalis muscle - aids in voluntary retention of faeces
Pelvic support muscles
These muscles act as the sling to support the organs of the pelvic cavity:
Coccygeus - elevates the pelvic floor
Iliococcygeus - elevates the pelvic floor
Levator ani - elevates the pelvic floor
Pubococcygeus - elevates the pelvic floor
Sexual performance related muscles
Urethral sphincter muscle - compresses the vagina
Bulbospongiosus - compresses the vestibular or clitoral bulb and constricts the vaginal orifice
Ischiocavernosus - compresses the corpus cavernosum of the clitoris, maintaining blood in erectile tissue
Pubovaginalis - draws the vagina forward and upward
Stability related muscles
Superficial transverse perineus - fixes and stabilizes the perineal body
Deep transverse perineus - fixes and stabilizes the perineal body
Internal obturator - laterally rotates and abducts the thigh
Piriformis - laterally rotates and abducts the thigh